What I Said Then:
Today marks 3 weeks since I first went to doctor at Christine’s urging with a cough. 3 weeks since I was told that that I have cancer.
I’m going to take a break here from the time-line of our riveting and unraveling blog saga to give some current news updates.
We finally received the pathology results back on Friday afternoon and it indicated that in fact I have Hodgkin’s Lymphoma (or Hodgkin’s Disease). We had initially been expecting a return of non-Hodgkin’s but in someways the actual diagnosis is better than the expected one. But in other ways it’s not.
For starters Hodgkin’s Lymphoma is one of the most curable forms of cancer. This is an important distinction to make, it’s not just treatable its one of the most curable forms of cancer. As in: one and done, if we get it now, and if stays away for a few years, it’s my understanding that there is something like a 90% chance that we’ll never, ever hear from it again!
Hodgkin’s most often strikes people in their late twenties or early thirties. Christine and I have already been introduced to 2 people our age who have already had Hodgkin’s Lymphoma (past tense). As we already know its very treatable, but one reason that it’s so treatable is because it tends to be a very aggressive form of cancer and as such responds well to treatment. The downside to this, is that since it is more aggressive, it must treated more aggressively. Rather than a 3 week cycle of chemotherapy, I can now look forward to a 2 week cycle.
I haven’t had the chance to get into the details of the chemotherapy cycle (and to be completely honest I hardly know myself what to expect at this point) but I know that every 2 weeks I’ll be going in for a dose of chemotherapy which is essentially a cocktail of several drugs given intravenously to attack and destroy cancer cells. It kills a lot of other cells in the process The body then spends the next two weeks “recovering” and rebuilding (read: mostly throwing up) and we start all over again. Huzzah!
I’m getting a little bit ahead of myself at this point, in terms of the planned narrative that was originally being laid out in these blog posts, but this next bit of news is sort of a game changer so I’m going to skip ahead a few days and try to catch everyone up to speed in order for this to make sense. (What I’m skipping is our first meeting with Oncologist and a few other interesting (or not) tests. At some point I’ll go back and tell those stories for the completion-ists out there who “gotta catch ’em all” and want the whole story)
So, on the Thursday following the Monday surgery I had what was is called a PET Scan. This is a test designed to visually show areas that are effected by cancer. This test takes advantage of the fact that cancer cells are highly metabolic (as does chemotherapy for that matter). Cancer cells can grow and divide up to 20 times faster than most other cells in the body. For the PET scan, I fasted for 12 hours and then had a radioactive glucose (sugar water) injected into me. The cancer cells absorb this glucose more rapidly than other cells and when the machine scans you it takes pictures of the radioactive areas of your body. In short, the areas of the body that are glowing brightly in the test results are cancerous.
The day after the test we received a call from the oncologist and the results of my PET scan (I haven’t actually had the chance to see them, but I hope I eventually will) were pretty much as expected. The tumor in my chest and the lymph nodes in my neck showed up the brightest. However, there was an area near my lower vertebrae that appeared in the test as dim glow. She indicated to us that this was unexpected, but that she wasn’t overly concerned about it as it didn’t look like the rest of the results. She felt that it was probably unrelated, but as it was important to get the full picture of what is going on in my body she ordered an MRI for me.
If anyone had MRI on their Cancer Test BINGO! Card, be sure to mark it off it now! To recap in order: X-Ray, CAT Scan, Lymph Node Biopsy, Bone Marrow Biopsy, PET Scan, MUGA Scan, and now an MRI!
The MRI took place just this Wednesday and took about 45 minutes. I understand that a lot of people can get very claustrophobic during this test and it’s easy to see why. But for me, I just had a hard time lying perfectly still for 45 minutes and got pretty fidgety during the last 15 minutes or so.
We got the MRI results at the same time that we learned it was Hodgkin’s Lymphoma. It turns out that the area which showed up dimly on the PET scan is in fact cancer. This involvement of the thoracic vertebrae means we’ve received FREE UPGRADE to Stage IV cancer, with all right and privileges!
The biggest change is that we can now expect that I’ll be receiving chemotherapy for 6-8 months (rather than the initial 3-4 that we were expecting with non-Hodgkin’s lymphoma) and additionally, like I said, I’ll now be doing chemo therapy treatments every 2 weeks. It’s faster, more intense, and longer. But it should have a better and more permanent outcome in the long run.
Finally, the last bit of news. I start chemo on Tuesday. But more on that tomorrow.
If you have any questions at all about this change of diagnosis, please feel free to contact me or ask them in comments below, and I’ll address them as I can.
What I Say Now:
Updated one year later – October 4, 2011
I remember EXACTLY where I was while I took that phone call from my doctor.
I was at home, and took the call sitting at the dining room table. Sitting on near the sliding glass door, with my back to the kitchen. The dog was outside, looking in at me.
I really didn’t react emotionally to the news because I was intensely focused on writing everything down and not missing anything (probably one of the reasons that I remember it so clearly. That, and it was a pretty momentous call). Normally I would rely on Christine in these moments, but she had only recently started going back to work, so I was on my own and I wanted to be sure that I didn’t miss any of the key new information that I was getting. And there was a lot of it.
New diagnosis. New treatment plan. A more aggressive staging. And some action items for me to do in order to make an appointment to have a chest port put in and to get chemo started.
After hanging up with her I called Christine. When she got home shortly thereafter we started making calls to the rest of the family. If I recall correctly, they all took copious notes on the new information as well.
This also marked a key moment in my Blogging. Up until that point I was speaking in the past tense about the events that happened in the previous weeks, but with the new information I switched into the present. Because of that, there were several things that I never wound up talking about, that I still need to go back and tell at some point: MUGA Scan, the Bone-Marrow Biopsy process, MRI, etc.
SO, it was a good deal of new information for everyone to wrap their heads around. But in the end it all wound up to be pretty good news. Yes, it was a more aggressive form of cancer. Yes, it had progressed farther than we thought. And yes, it would be a longer and more frequent form of chemo. BUT (and this was and still is a big “BUT”) I now had a shot at getting into that club of over 88% of the people who are diagnosed with Hodgkin’s and beat it.
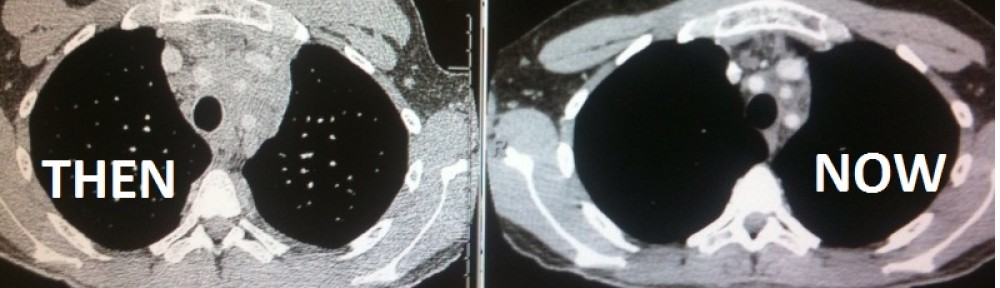
So far, so good! As of this writing I had 2 of my “every 3 month” follow-up CT Scans. I’m on my way!