What I Said Then:
Lets start at the beginning.
In hindsight, it all started with a cough. It was the cough that showed up first, and a few months later, it was the cough that finally convinced me to go see a doctor. When I called the doctor last Monday I told them that I wanted to be seen for what I could only describe as a “persistent, non-productive cough that I’ve had for about 2 months.” I first took notice of my cough, during tech rehearsals for a small fringe-theater show I was doing. In general I’d be fine during the day, but when I would arrive at the theater every night this cough would show up, and then would peak as I was going to bed. I clearly didn’t have a cold or anything as there was never any mucus or anything associated with the cough. I would just get to the theater in the evening and would basically cough and hack my way through the show while I was backstage. I could control it while I was onstage, but all evening I there would be this weird irritation in my lungs that would make me have to cough.
We did that show at the Center House Theater, which is an old musty space, so my initial instinct was that there was something in the space that I was reacting to. I tend to have allergies to molds and things, so I just assumed that there was mold in the space and that was why I was coughing every evening. After the show closed and I still had the cough hanging around I started to assume that perhaps it wasn’t mold at the theater, but mold in our house. It was at about this same time that the summer was finally starting to show up so we began using the air conditioning regularly and I thought, well looks like there is something in our central air system here in the house that I’m reacting to. After all Christine wasn’t sick, and if it was some kind of disease wouldn’t Christine have contracted it by now?
As one show came and went and I transitioned to my second gig for the summer, the cough stayed. Always there, always just in the background and in the back of my mind. The pattern stayed the same. I was fine for most of the day, it would pick up in the evening, and then going to bed would be a production as laying down would always aggravate that pesky cough. I started to think that there might be some fluid in my lungs. It wasn’t coming up at all, but maybe that’s why it’s worse when I lay down? The mold theory was still in full effect too. We did that second show in a another small basement theater with low air circulation, so there could have been molds and such in that space too (or so I thought).
Further perpetuating the theory that it was environmental irritants that were making me cough was the fact that during the latter half of our August trip to Hawaii my cough went away for a few days. It was there for the first half, I remember promising Michele and Eric (who we were traveling with) that I wasn’t contagious as I would hack and cough around their 1 year old son. But it didn’t go away permanently, as it returned during the run of that 2nd show shortly after our vacation.
I don’t want to paint an inaccurate picture here. I wasn’t coughing all the time, I would just have several coughing fits throughout the day. It was just enough to notice that you still had that cough, and just enough for Christine to bug me for several weeks about making a doctor’s appointment.
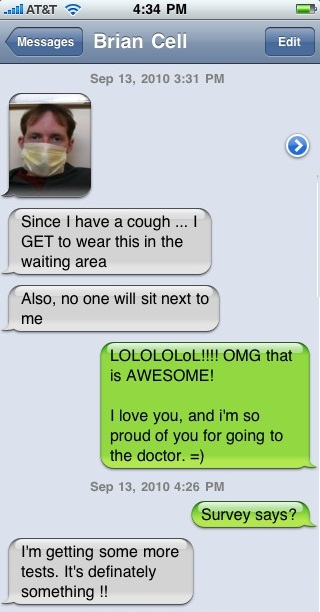
When I checked in at the doctor’s office, they saw that I reported a cough and so they made me wear a mask in the waiting room. I was already pretty unamused at the fact that I was here so I took this picture and I texted it Christine.

- Unamused Brian is unamused
What you need to realize is that the last time I went to see a doctor for something like this it was my pediatrician. I don’t care for doctor’s offices, and frankly I’d never been the person who gets sick a lot or needs to go to the doctor for a cold or slight flu. So for me to even be here was a big deal and kind of a huge annoyance to me. And now I had to wear this mask, and to make matters worse, no one would sit next to me in the waiting room.
I was called back to the exam room, and before I even saw the doctor, he had me go in for a chest X-ray, just based on my “persistent, non-productive cough that I’ve had for 2 months” that I told them when I called to set up the appointment. After the X-ray I went back to the exam room and waited a few minutes. When the doctor came in he told me that I could take my mask off and that knew why I was coughing. I didn’t fully grasp the gravity of what he was saying at the time, though I kind of thought I knew where it was going when he cut to the chase and opened with: “The X-Ray doesn’t indicate any signs of infection in your lungs, but there does appear to be a mass in your anterior mediastinum.” To which I replied: “Great! That’s one of my favorite Steinem’s, right behind Gloria.”
Hi, I’m Brian, and I make jokes when I’m uncomfortable.
He was indicating to me that I had a serious medical condition, and I came back with a joke. Not what he expecting, and it took him a few seconds to regain his professional composure after a good laugh. But at least we understood each other now.
I should tell you at this point, that in the end, it wasn’t just the cough that finally made me think it might be a good idea to see someone. There was a handful of other things which (like the mold theory for the cough) I had perfectly good justifications for. But when I started thinking about them all together I realized that there was a chance that I was actually looking at a short list of symptoms.
As it turns out, if you Google non-Hodgkin’s lymphoma symptoms you’ll get a list a looks very similar to this:
- Fever
- Drenching night sweats
- Weight loss
- Fatigue
- Loss of appetite
- Severely itchy skin, often affecting the legs/feet
When the doctor and I sat down and started talking I pretty much went straight down that list and hit each and every point on it with little or no prompting or questions from him. And with most of them I even had a reason for why I had dismissed it.
Fever: I had a fever of about 100 when I checked in to the doctor’s office, and I assumed that I had been running a low-grade fever for a while, but that wasn’t so surprising to me. By the time I went to the doctor I was pretty much willing to admit that I was sick. But I just thought it was something mild.
Night Sweats: For most of the summer it was it was not uncommon for me to wake up two or three times a week completely drenched and dripping with sweat. But it was summer, it’s hot out, and I can’t sleep without covers on me so I didn’t really think much of it. Additionally Christine had bought a new comforter for the bed at the beginning of summer, so I have been bitching to her for months that “this this doesn’t breathe!” (For the record, she maintained that it breathes just fine.)
Weight loss/Loss of appetite: I actually blogged about this several months ago. We have really tried to make some major changes in our diets over the last few months by switching to mostly local and organic foods. The result of which I assumed (and as I wrote about) was that I was eating much more wholesome and fresh food. As such I wasn’t eating as much and I was less, since my body was getting was it needed (or so I assumed) and it lead to a natural weight loss. Though I do have to admit that recently I was a bit surprised. I’ve always been pretty scrawny, and I normally walk around at about 145-150. But at one point a few weeks ago I stepped on the scale and saw 134 (I’m 5′ 11″ BTW) That was a bit surprising, but even then I’ve been that skinny before. I even had a conversation a few weeks ago with some cast-mates and we talking about weight and I mentioned that I was oddly back at the weight I was at when I graduated High School, even without exercise. =)
Fatigue : Not something I put too much stock in at the time, but I have certainly been tired a lot lately. Sleeping in, AND I could think of several instances in the last month where I had taken a nap in the middle of the day, which is completely unheard of for me. Still, I keep waking up because it’s so hot at night, so maybe I’m just not sleeping well =)
Severely itchy skin, often affecting the legs/feet : The easiest of all the symptoms for me to dismiss. I have always had a pretty serious grass allergy, but this summer I fell in love with sandals (Tiva’s) for the first time and everyday I would walk around in the backyard while playing ball with dog. So that would explain why my ankles are pretty much scarred from me scratching them mercilessly all summer. Additionally I’ve taken up Golf pretty seriously this summer and have played quite a bit. I even had a conversation with Dane (one of my golfin’ buddies) earlier this summer about how badly my ankles and feet had been itching because I have grass allergies and how it’s especially bad by the time we get to the back 9.
Each thing alone seemed pretty benign. But when I thought about them together, even I had to admit that I was probably sick. But even then, when I went to the doctor on Monday the 13th, I thought for sure he was going to tell me that I had walking pneumonia or a low-grade infection of some kind. No one suspects the Spanish Inquisition cancer. Except for my doctor of course… he pegged it right away.
After we talked he gave me a physical examination. He noted that the lymph nodes in my neck were severely swollen and I told him that they had been for sometime now (afterward I remembered back to one of my costumes, I remembered how I wasn’t always able to button the top button of my shirt because it put uncomfortable pressure on my neck, but not always). He completed the physical examination and we sat back down he typed a few things into the computer, turned to me and gave it to me straight.
“I see no reason to sugar-coat this, I believe that you have non-Hodgkin’s lymphoma.”
It’s always interesting to see how someone responds to frank bad news (we’re getting pretty used to dishing it out lately) but I even managed to surprise myself with my immediate and enthusiastic/sarcastic response:
“Great! Just what I’ve always wanted!”
As I understand it now, aside from the swollen lymph nodes, most of the symptoms aren’t really the symptoms of lymphoma itself. But as the cancer spreads outside of the lymphatic system, the body starts to loose its ability to fight infection and these tend to be the most common side effects of that. In my case it all comes back to that “mass in your anterior mediastinum.” The cough comes from the mass (or tumor) pushing back against my lungs and trachea as I breath in. The tumor is also responsible for the other side effects, both as the body attempts to fight it and as it throws off various chemicals and whatnot as it grows.
What even more interesting is that we’ve since learned that the tumor is necrotic. Cancerous cells are highly metabolic. They divide, and grow up to 20 times faster than normal cells in the body. In this case the tumor grows and swells rapidly until it quickly out outgrows it’s blood supply, at which point it starts to die and shrink back before the process repeats again. Right now the mass in my chest is in a necrotic stage and is slowly shrinking.
The most terrifying thing about all of this is that in the last week all of the symptoms that I’ve talked about, the cough, the night sweats, the fever, practically everything has completely disappeared. Gone. If I had waited a couple of more days before finally deciding to go to the doctor I wouldn’t have called. It’s unclear what sort of time frame this tumor would continue to cycle on, but to me it seems possible that had I not gone to the doctor it could have been a while before these symptoms came back and all the while the cancer would be continuing to spread and take hold in other parts of my body. I shutter to think at what stage it might have been at the next time I started to feel symptoms. It’s a sobering thought.
Back in the doctor’s office: So, there I was. I had reluctantly gone to the doctor for the first time in 20 years. I’m 28 years old and the doctor just told me that I have cancer. On my way out of the clinic I stop at the lab for a blood draw (again, my first in 20+ years). Then I get in the car, head to the Post Office to mail some packages, and then I head home and wait. Christine was due home in about 20 minutes, and we were about to start officially dealing with this news.
What I Say Now:
Updated 1 year later – September 29, 2011
One the most remarkable aspects of this story turns out to be the speed at which I was “diagnosed.” I walked into the doctors office and less than hour later the doctor said those words which are now burned into my memory “You seem like a fairly straight-forward guy, so I don’t see any reason to sugar coat this: I believe that you have non-Hodgkin’s lymphoma” (HA! The joke’s on YOU Dr. Dodge, it was HODGKINS Lymphoma …)
I have since met several people my age who have been diagnosed with Hodgkin’s Lymphoma and most of them went through a fairly long (often over a year) series of referrals and doctors visits. They would go to the doctor because they didn’t feel good, or just didn’t feel quite right, so there isn’t much the doctor can test for. Or maybe they went in for that slight cough and lethargy and then get sent to a ear, nose, and throat doctor or something like that. Then maybe they get put on a steroid, or tested for asthma. Then (as happens with these necrotic tumors) when cough goes away, you’re cured! Or at worst, you stay on those asthma drugs for a while.
I’m sure the stories are out there, but I have yet to hear another diagnosis story like mine. Maybe it was the way I described my ailment when I called, but for whatever reason, the doctor read that I had a “persistent, non-productive cough that I’ve had for about 2 months.” and BEFORE HE EVEN MET WITH ME, had me take a chest x-ray which showed the tumor in my chest.
As we were walking out the door together, the doctor asked me if I wanted him to call and help me tell my wife. I declined and after he had asked several times if I wanted him to call that night I agreed it might be a good idea. I’m pretty sure that I stopped being able to fully listen to what he was saying after he told me I had cancer, and I was sure that Christine would have questions that I hadn’t thought to ask.
Like I said in the original post, after leaving the doctor’s office I went to the Post Office. As a part-time eBay seller it’s a place I’d been hundreds of times before, but obviously this time it felt a little different. Right away I realized that things were different, and were possibly never going to be the same. Now that I knew I was sick, I felt sick, and it was more than just the shock I was in. Again, this was a place I go to almost everyday at this time, but now it felt like an out-of-body experience. Am I really here? Did that appointment really just happen? Can these other people in line tell that I’m sick? AM I really sick? Maybe the doctor was wrong. This can’t be happening … “Uh… yeah, First-Class International please…”
I drove home, still very much in that distracted out-of-body state. My brother-in-law (who was staying with us for the summer) was on the couch playing video games. It was a routine Monday afternoon for him, not so much the life-changing afternoon that I just had. I have NO memory of anything that happened during the next 30-45 minutes while I waited for Christine to come home. I probably just sat there in shock, and running possible scenarios in mind for how I was going to tell her.
She came in, excited that I had finally gone to the doctor, and eager to hear what the doctor said (especailly since I think she was excited to see if she was right to suggest I go in =) She had texted me earlier and this is a screenshot from her phone:
I apparently over-played my hand with my use of exclamation marks. I was trying to be fun, so as to not alarm her too much. But apparently she knew something was up by the way I responded with punctuation. To quote her just now: “Yes, you only use punctuation when you’re drunk or upset about something”
I told her that the doctor that gave it me straight, and so I was just going to do the same thing for her. And I said out-loud for the first time the same opening line that I would soon repeat to the rest of my family. “He told me that I have non-Hodgkin’s lymphoma… which is to say, that I have cancer”
Dr Dodge was right, and we were both thankful for the phone call that he gave us from home a few hours later, he was able to help talk Christine off the ledge and it was helpful that he reiterated some of the same “life-changing, not life-ending” points that I had told her. The rest of that night though was a flurry of emotions and I don’t recall many specifics moments, mostly just what I wrote in the next post. By the time we went to bed at like 10 or 10:30 we were pretty exhausted.