… but I’m starting to lose the battle against chemotherapy.
Every time I go in for chemo I am asked the following questions:
Are you having any pain?
Experiencing increased fatigue?
Any shortness of breath?
Coughing?
Numbness or tingling in your extremities?
I always get the feeling that they are looking for something, almost waiting expectantly for me to answer to yes to one of those of those questions. Expecting complications.
I finally had to answer “yes” when we last met with the oncologist on Wednesday. I actually reached out to my doctor regarding shortness of breath about 2 weeks ago. What I first started noticing was that my body was acting like it wasn’t getting enough air. Even if I was just sitting on the couch I’d find an increasing need to to yawn, or take a deep breath from time to time. I also noticed several instances where I would wake myself up in the middle of the night with the need to take a deep breath. My doctor didn’t seem concerned about it at the time, but told me to keep an eye on it.
Over the New Year weekend I started to notice an increase in the “shortness of breath” that I’m asked about every two weeks. I would notice it particularly when getting up and moving around after sitting for a long period of time. I started getting winded pretty easily and then when I would take a deep breath, the last bit of it felt as if I was smoking a cigarette. That’s kind of the only way I know how to describe it. I’ve never been a “smoker”, but I’ve smoked cigarettes in my life, at parties in college or whatnot. That feeling of breathing in smoke when you’re body is expecting air is a very distinct and odd feeling for a non-smoker and over the next couple of days I started to notice it more and more. The slight burning sensation in my lungs, and the feeling that no matter how big a breath I was taking, it didn’t seem to benefit me more than a regular or shallow breath. They felt the same. It’s as if that extra bit of lung capacity isn’t there.
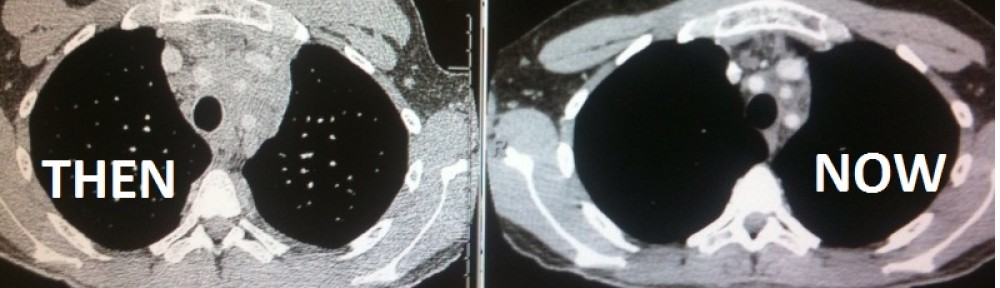
Lung damage, though not common, is not totally unexpected with the treatment course of ABVD chemotherapy that I’m on. It’s the “B” that does it. Bleomycin can attack the lungs and in some cases cause permanent lung damage. It’s too early to speculate that any possible damage done my lungs (if that’s what is happening) at this point is permanent, but it does exist within the realm of possibilities. Again, we are dealing with some seriously potent drugs here.
I don’t think I ever mentioned it here, but before starting this treatment course I was given a lung function test both as a measure of health before starting chemo (to ensure my lungs were healthy enough given these known risk factors) and as a baseline for any possible complications. Later this week I’ll be going in to repeat this test now that I am beginning to show symptoms of possible lung damage. It’s a simple sit here, hold your breath, blow into the tube kind of test. The last time I took it, it was actually pretty tough since I still had a large tumor pressing back on my lungs, but after a few failed attempts to make it through the steps without coughing, I got through it.
As a precaution, I was taken off of the bleomycin for this cycle of treatment. Meaning that they only gave me 3 of 4 drugs that I normally receive every two weeks. After the results of this week’s test they’ll take a look at my lung function and decide if and when to put me back on it. In the mean time I’m just trying to breath normally =) Fortunately I haven’t felt the shortness of breath as acutely when just walking around like I did toward the beginning of last week, but I do still feel it when exert myself. On the plus side, if my lungs are being effected by the drugs I feel that we definitely caught it in the early stages.
I’ve talked about it again and again, but I still have problems wrapping my mind around just how sick the “treatment” for cancer can make one. So once again, if I haven’t made my official position on the subject known, then let me say: if you are ever given the choice between getting cancer and NOT getting cancer, I would advocate for “NOT getting cancer.” If it’s one thing you take away from being a reader of my blog, I hope it’s that!